Introduction: Nucleolar spindle-associated protein 1 (NUSAP1), a microtubule binding protein with molecular weight of 55KD, plays an important role to ensure the normal regulation of cell cycle in chromosome separation, spindle assembly and DNA repair. NUSAP1 has been shown to be highly expressed in a variety of tumors, involved in tumor occurrence, invasion, migration, and drug resistance. Moreover, it is associated with poor prognosis. Whereas, no research has been reported regarding the role of NUSAP1 in diffuse large B-cell lymphoma (DLBCL).
Methods: Peripheral blood samples from de novo DLBCL patients and healthy volunteers were collected with informed consents at the Department of Hematology in Shandong Provincial Hospital Affiliated to Shandong University (SPHASU). Microarray datasets GSE83632 and GSE32918 were obtained from Gene Expression Omnibus. Kaplan-Meier survival curves with log-rank test of overall survival (OS) were analyzed. Immunohistochemistry staining (IHC) was performed to assess NUSAP1 expression in specimens. Expression levels of NUSAP1 mRNA and protein were detected by quantitative RT-PCR and western blotting. The DLBCL cells were transfected by lentiviral shRNA and vectors to stably silence and up-regulate NUSAP1. Effects of doxorubicin on cell viabilities were assessed by cell counting kit-8. Besides, apoptosis and cell cycle were respectively detected by annexin V-PE/7AAD and PI/RNase staining via flow cytometry. Invasion ability was analyzed by transwell assay. ShNUSAP1 cells and Scramble cells were subcutaneously injected to SCID-Beige mice to establish xenograft models. Animal experiments were performed in accordance with the principles of the Institutional Animal Care.
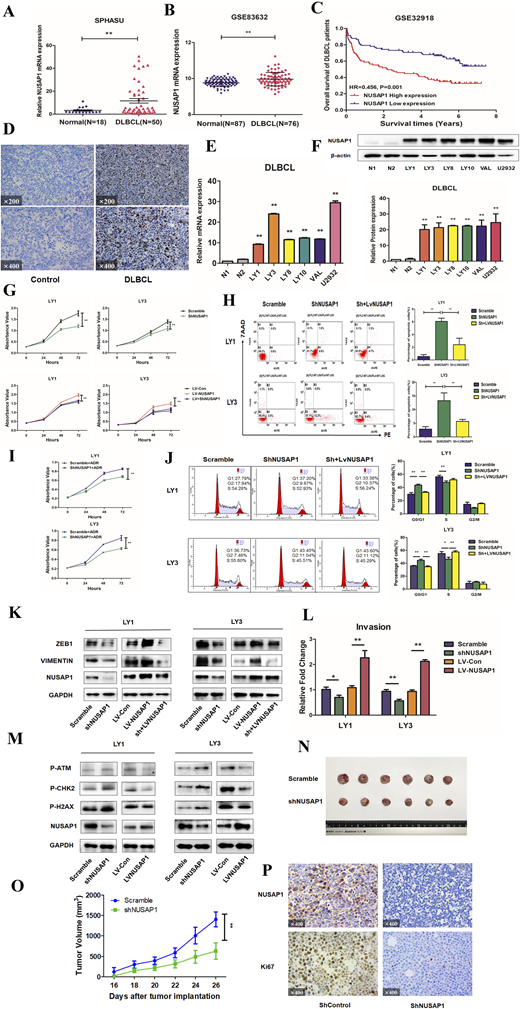
Results: According to clinical specimens and bioinformatics analysis, the expression level of NUSAP1 gene in samples of DLBCL patients was significantly increased than that of healthy donors (P<0.05) (Figure A, B). Besides, patients with high expression of NUSAP1 was related to shorter overall survival (HR=0.456, P<0.01), indicating poor prognosis (Figure C). Stronger positivity of NUSAP1 was markedly observed in DLBCL lymph nodes than reactive hyperplasia group, which was associated with Ann Arbor stage of DLBCL patients (Figure D). Compared with normal B cells, both the mRNA and protein level of NUSAP1 were up-regulated in DLBCL cell lines (Figure E, F). After transfected with lentivirus, the proliferation rate of NUSAP1 knockdown group was lower than that of the control group, while the overexpression group was faster than control (Figure G). Through flow cytometry, silencing of NUSAP1 led to increased apoptotic rates of LY1 and LY3 cells (Figure H). Along with the recovery of NUSAP1 expression level, apoptosis rates were improved again. With the addition of doxorubicin at 100nM, interference of NUSAP1 could increase the sensitivity of cells to doxorubicin (Figure I). NUSAP1 intervention induced obvious cell cycle arrest in G1 phase of LY1 and LY3 cell lines, with concomitant reduction of cell proportion in S phase (Figure J). Moreover, known as EMT biomarkers, the expression of ZEB1 and VIMENTIN were decreased with reduction of NUSAP1. Likewise, we also investigated NUSAP1 overexpression has promoted EMT-like process of LY1 and LY3 cells (Figure K). Surppression of NUSAP1 inhibited the action of DNA damage repair pathway (Figure L). Moreover, we also found that NUSAP1 knockdown induced striking reduction in invasion cells (Figure M). We found that tumor growth was significantly suppressed by inhibiting NUSAP1 in xenograft models (Figure N, O). IHC for NUSAP1 and Ki67 on tumor sections showed that tumors derived from shNUSAP1 cells exhibited significantly lower levels of Ki67 compared to control group (Figure P).
Conclusions: This study first identified that the high expression of NUSAP1 in DLBCL patients is associated with poor prognosis through database analysis and in vitro experiments. Interference of NUSAP1 expression led to a slower DLBCL cell proliferation and a higher apoptosis rate, meanwhile induced the G1 phase arrest and promoted EMT-like process. Collectively, our study demonstrated that NUSAP1 plays a role in promoting tumor growth both in vivo and vitro through DNA damage response pathway, which providing a new direction for prognosis assessment and targeted therapy of DLBCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal